In
an article I recently read, Viatcheslav Wlassoff explains that Post-Traumatic
Stress Disorder is triggered by experiencing a traumatic event, such as war
violence, rape, child abuse, or near death experiences, among other experiences.
In cases of PTSD, the emotional wounds linger and it results in symptoms such
as flashbacks of the traumatic event, severe anxiety, hypervigilance, and more.
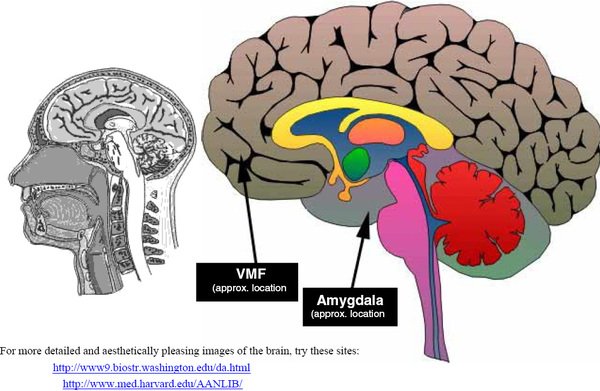
He explains that PTSD actually changes the brain’s structure, namely the
circuit involving the ventromedial prefrontal cortex (vmPFC) and the amygdala.
Neuroimaging
studies have shown that specific parts of that circuit, such as the vmPFC and
the amygdala, differ structurally and functionally in PTSD patients, compared
to healthy individuals. Specifically, in Wlassoff’s article, he explains how in
PTSD, changes in the vmPFC such as reduced volume of the cortex, along with its
decreased function ability, have been shown. He explains that the vmPFC is the
part of the brain that is responsible for regulating the emotional responses
that are triggered by the amygdala.
He
also explains how traumatic experiences appear to increase activity in the
amygdala, and that PTSD patients show hyperactivity in the amygdala in response
to stimuli that are related to their traumatic experiences.
This
prevailing neurocircuitry model explains the stimulus in our environment is
capable of inducing fear by triggering activity in the amygdala, which in turn
triggers the physiological and subjective experience of fear. Neuroscientists have
come to believe that activity in the amygdala is regulated by the vmPFC, and
this has been shown by many studies, such as anatomical tracing studies in
primates that have shown very dense projections from the vmPFC to the amygdala.
Dr.
Michael R. Koenigs, who came to talk at our Neuroscience Seminar this
semester, also described other studies that have also shown how vmPFC activity
is inversely related to amygdala activity, but that this is not necessarily the
case with people suffering from depression. He therefore shed light on the fact
that although the vmPFC is important for coordinating activity across a complex
network including the amygdala, the conventional neurocircuitry model of vmPFC
function is incomplete.
Koenigs
demonstrated this by discussing the findings of several studies. For example,
he studied American combat veterans who fought in the Vietnam War, including
ones with brain damage. Amongst the people he studied with vmPFC damage, he
found that these subjects were actually less likely to suffer from depression.
Furthermore, he discussed another study of a 30 year old woman who suffered
from severe depression for more than 10 years. The woman attempted suicide with
a gunshot to the head, and although she survived, damaged her entire vmPFC.
After the attempt, she showed no signs of depression whatsoever.
These
studies demonstrate that although it is known that vmPFC and amygdala
dysfunction is related to symptoms of PTSD, saying that it it is only these two
factors, and that these work in a causal manner to bring about PTSD symptoms,
would be incorrect. The studies Koenigs discussed have shown that we still have
a lot more research to do to fully understand the neurobiology of psychiatric
disorders such as PTSD.
Works Cited
Wlassoff, Viatcheslav. "How Does Post-Traumatic Stress Disorder Change the Brain?." Brain Blogger. N.p., 24 Jan 2015. Web. 06 Dec. 2015. <http://brainblogger.com/2015/01/24/how-does-post-traumatic-stress-disorder-change-the-brain/>.
Koenigs,
Michael. "Revising Neurocircuitry Models of Mood and Anxiety
Disorders Based on Evidence From Brain Lesion Patients and Psychopathic Criminals."
Neuroscience Seminar. Loyola University Chicago, Chicago. 10 Nov. 2015. Speech.


Assignment Help At Sin-compromiso
ReplyDeleteAssignment Help At Tec
Treat Assignment Help
Assignment Help At Ligue-Cancer
Online Assignment Help UK
Geography Assignment Help UK
Economics Assignment Help
TreatAssignmentHelp - An Assignment Writing Company in UK
Treat Assignment Help By GeorgiaStewart
Treat Assignment Help By AnaGibson