The
Challenges of Current Prosthetics
In a recent study at the Rehabilitation Institute of
Chicago, Kuiken et al. (2007) conducted an investigation that used targeted muscle
reinnervation as a way to improve the function of prosthetic arms. Kuiken and
colleagues (2007) developed the targeted muscle reinnervation method as a way
to solve some of the difficulties with current prosthetics, and overall
increased motor skills for individuals
with amputated limbs
What is TMR?
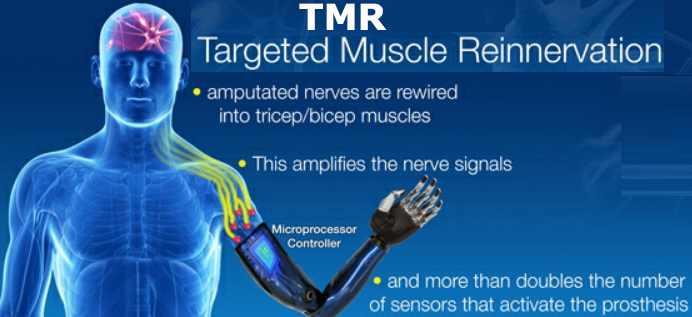 To begin with, the goal of this
experiment was to develop new motor and sensory signals in the chest as
a way to provide sensory feedback for a missing limb. The method used by Kuiken
and colleagues (2007) to accomplish this was targeted muscle reinnervation
(TMR). This approach transfers functional nerves from the amputated
limb and sews them together into a larger group of muscles that are located in
the chest. In the case explained by Kuiken et al., the ulnar, median,
musculocutaneous, and distal radial nerves were removed from the amputated
limb, and places into the pectoral muscles of chest. The neural connections to
the brain still exist in the pectoral nerves, but since the distal ends of
these nerves are missing (located in the amputated limb), the pectoral muscles
remains non-functional. Think about how
difficult it must be to want to make a fist with your hand but not have
any fingers. The neural connections are still there, the forearm muscle will
contract but there is no end point because there is no hand. With the TMR technique, the motor
nerves from the amputated limb are sewn together with the remaining pectoral
muscles. The pectoral muscles will act as neural amplifiers for motor control
and are necessary for this experiment because they have the established neural
connections to the brain. (Kuiken et
al., 2007) Although the TMR method may seem very complex and slightly remind
one of Frankenstein, the results for targeted muscle reinnervation have been
able to return many fine motor skills to the patient at a rate that is four times faster than the
normal prosthetics. This is because the pectoral muscles with the neural
connections have been connected to neurons that control fine motor skills. With
the attachment of a modified prosthetic, the patient will think about making a
fist, the message will travel through the neural pathways to the pectoral
muscles, that now have fine motor nerves attached to them, and synapse on
specialized electrode located in the prosthetic. The electrode will encode the neural activity into the prosthetic, and the action will terminate with the prosthetic making a fist.
To begin with, the goal of this
experiment was to develop new motor and sensory signals in the chest as
a way to provide sensory feedback for a missing limb. The method used by Kuiken
and colleagues (2007) to accomplish this was targeted muscle reinnervation
(TMR). This approach transfers functional nerves from the amputated
limb and sews them together into a larger group of muscles that are located in
the chest. In the case explained by Kuiken et al., the ulnar, median,
musculocutaneous, and distal radial nerves were removed from the amputated
limb, and places into the pectoral muscles of chest. The neural connections to
the brain still exist in the pectoral nerves, but since the distal ends of
these nerves are missing (located in the amputated limb), the pectoral muscles
remains non-functional. Think about how
difficult it must be to want to make a fist with your hand but not have
any fingers. The neural connections are still there, the forearm muscle will
contract but there is no end point because there is no hand. With the TMR technique, the motor
nerves from the amputated limb are sewn together with the remaining pectoral
muscles. The pectoral muscles will act as neural amplifiers for motor control
and are necessary for this experiment because they have the established neural
connections to the brain. (Kuiken et
al., 2007) Although the TMR method may seem very complex and slightly remind
one of Frankenstein, the results for targeted muscle reinnervation have been
able to return many fine motor skills to the patient at a rate that is four times faster than the
normal prosthetics. This is because the pectoral muscles with the neural
connections have been connected to neurons that control fine motor skills. With
the attachment of a modified prosthetic, the patient will think about making a
fist, the message will travel through the neural pathways to the pectoral
muscles, that now have fine motor nerves attached to them, and synapse on
specialized electrode located in the prosthetic. The electrode will encode the neural activity into the prosthetic, and the action will terminate with the prosthetic making a fist.
Furthermore, a similar but different
method used by the investigators was targeted sensory reinnervation (TSR). The TSR method was done by placing some sensory
nerves from the amputated limb in the TMR area. The results showed that TSR
also brought back some of the sensations that had been lost such as: pressure,
temperate, and texture. (Kuiken et al., 2007) Moreover, the implications of
these findings have opened up new doors in the world of prosthetics. Now that the neural connections have been
properly established prosthetics must also be adapted with new myoelectric
signaling pathways. In all, it is clear that Kuiken and colleagues (2007) have
revolutionized the world of prosthetics, and neuroscience.
New Doors
Moreover, it is not just scientists
at the Rehabilitation Institute of Chicago that are working on improving
prosthetics, but also researchers at Case Western Reserve University. In the
article, A Prosthetic Hand That Can Feel, by Andrea Tsai and Alexandra
Sifferlin, the journalists explain the technological advancements being done at Case
Western Reserve University.
The obvious goal for these scientists
is to develop a prosthetic hand that can feel, and has a natural intuitive
sensation to it. Similar to the Kuiken et al., TSR technique that brought
back some sensory sensation, the researchers at Case Western have worked on a sensory approach of their own. In the Case Western
approach the prosthetic hand is equipped with specialized sensors that measure variations of pressure. The
sensors convert the mechanical stimulus into a neural message that it sent
through wires up to electrodes that have been surgically implanted in forearm
or upper arm (distal end of the body where limb was amputated). The electrodes encoded message into a neural message that is transmitted to
healthy neurons with established connections, that send the message to the
brain. (Tsai & Sifferlin 2015)
Compare and Contrast
Although very similar Kuiken et
al., and the researchers at Case Western seem to be approaching the problem of
prosthetics from different angle. Kuiken and colleagues were focused on
motor function that is controlled from the brain to the hand. TMR is connecting
muscles to muscles, and involves a prosthetic that can transfer the message
from the neurons to the hand, so that the prosthetic can execute the command.
They also performed TSR, except because the sensory nerves were sewn into the
pectoral muscles; the chest is the area that can feel. Think about it this way,
poking someone in the chest may feel like to the patient that you are touching his
or her right finger. Interestingly enough, the researchers at Case Western are working
on a different approach that goes from the prosthetic to the brain instead. Case Western has specialized sensors that encodes the information
to electrodes, which transmits the information to neurons and the brain. In the future, the researchers at Case Western hope to create a wireless system for their prosthetic. Wouldn't it be crazy for patients to control motor movements through the wifi?
If only the both approaches could be
implemented together this would create a new frontier for the world of
prosthetics.
Bibliography:
Kuiken, T. A., Miller, L. A.,
Lipschutz, R. D., Lock, B. A., Stubblefield, K., Marasco, P. D., Zhou, P.,
& Dumanian, G. A. (2007). Targeted reinnervation for enhanced
prosthetic arm function in a woman with a proximal amputation: a case study. The Lancet Journal, 369, 371-380. doi:10.1016/S0140-6736(07)60193-7.
Tsai, Diane, and Alexandra Sifferlin. "A Prosthetic
Hand That Can Feel." Time. Time, 16 Nov. 2015. Web. 01 May 2017.
Images:
http://www.industrytap.com/wp-content/uploads/2013/04/trm-2.jpg
http://mediad.publicbroadcasting.net/p/shared/npr/styles/x_large/nprshared/201411/358354216.jpg
http://www.clipartkid.com/images/73/frustrated-face-clipart-ELtksx-clipart.jpg

No comments:
Post a Comment